Student Research Symposium Program Portal: Submission #144
Submission information
Submission Number: 144
Submission ID: 8992
Submission UUID: 9f522cda-ec9d-46d4-9616-b835590941fa
Submission URI: /student-research/symposium/research-symposium-program-portal
Submission Update: /student-research/symposium/research-symposium-program-portal?token=KWuqPDGldqa6_e8xuE_jLWLvS2koh26wlyzrUyXZqGU
Created: Mon, 01/12/2026 - 03:25 PM
Completed: Mon, 01/12/2026 - 03:36 PM
Changed: Mon, 01/12/2026 - 03:36 PM
Remote IP address: 2600:1700:4400:1cc0:2ca3:2bfa:471f:892
Submitted by: Anonymous
Language: English
Is draft: No
Webform: Research Symposium Program Portal WF
Submitted to: Student Research Symposium Program Portal
Lindsey
Thorpe
{Empty}

Doctor of Nurse Anesthesia Practice
Kaitlin Gallagher is from Vero Beach, Florida. An outdoor enthusiast with four years of neuro ICU critical care experience, she is drawn to a wide range of anesthesia specialties—from obstetrics to neuro and thoracic anesthesia—and is completing her third degree at Florida State University.
Hannah Pimentel, from Normandy, Tennessee, is a registered nurse with seven years of experience. She has a strong interest in geriatric care and vulnerable populations and aspires to participate in a medical mission trip to deliver healthcare to underserved communities.
Lindsey Thorpe is from Palm Harbor, Florida. She has ten years of nursing experience, including three years as a travel nurse, and has a strong interest in cardiothoracic anesthesia.
Andrew Trainor is originally from Kansas City. He has enjoyed the opportunity to travel across the country to engage with new colleagues and patients while learning to be a nurse anesthetist along the way.
Hannah Pimentel, from Normandy, Tennessee, is a registered nurse with seven years of experience. She has a strong interest in geriatric care and vulnerable populations and aspires to participate in a medical mission trip to deliver healthcare to underserved communities.
Lindsey Thorpe is from Palm Harbor, Florida. She has ten years of nursing experience, including three years as a travel nurse, and has a strong interest in cardiothoracic anesthesia.
Andrew Trainor is originally from Kansas City. He has enjoyed the opportunity to travel across the country to engage with new colleagues and patients while learning to be a nurse anesthetist along the way.
Esophageal vs Nasal Temperature Probes: A Quality Improvement Initiative to Reduce Intraoperative Hypothermia
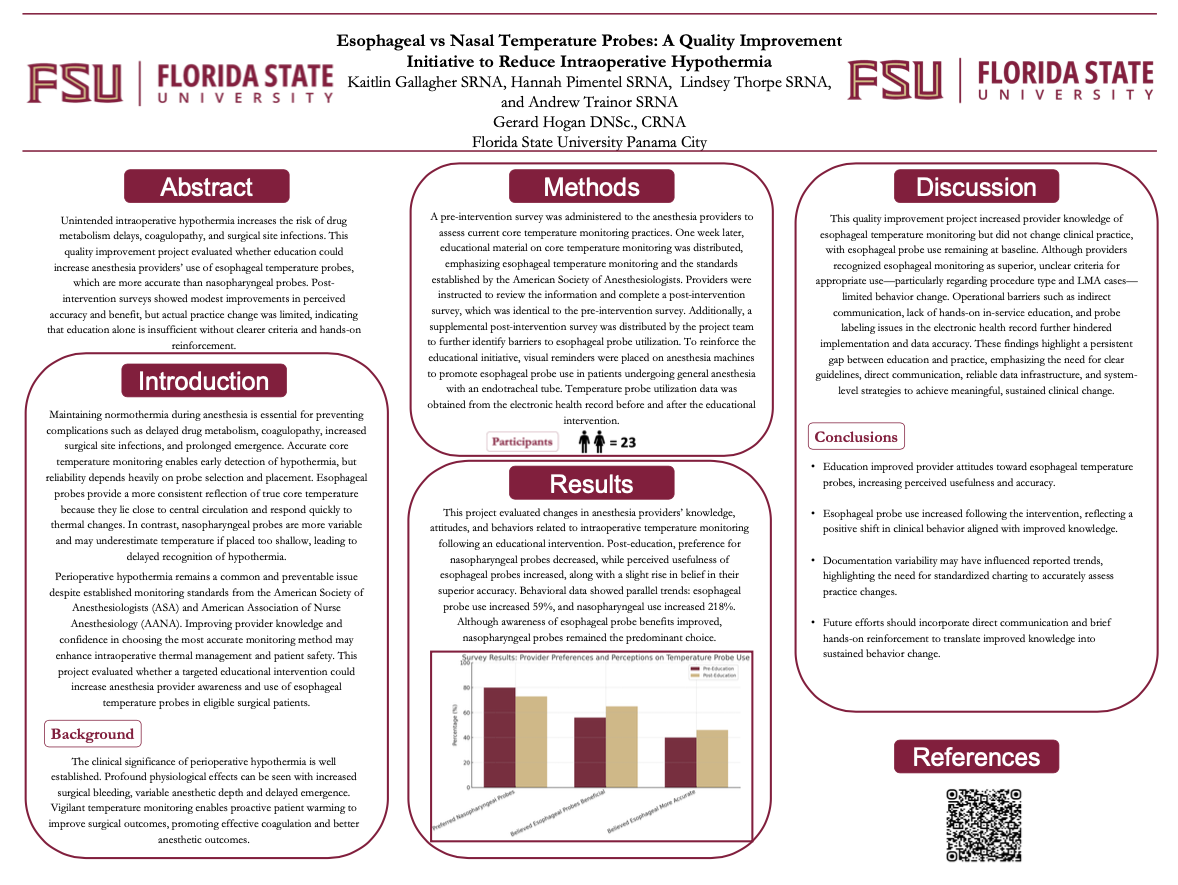
Unintended intraoperative hypothermia is a frequent anesthesia-related complication associated with delayed drug metabolism, coagulopathy, and increased surgical site infections. Accurate core temperature monitoring is essential for prevention, yet probe selection significantly influences measurement reliability. Evidence supports esophageal temperature probes as a more accurate reflection of core body temperature compared to nasopharyngeal probes, offering earlier detection of hypothermia and improved thermal management. This quality improvement project aimed to evaluate whether an educational intervention promoting the use of esophageal temperature probes among anesthesia providers would reduce the incidence of intraoperative hypothermia in adult surgical patients receiving general anesthesia. Conducted at a large community hospital in northeast Florida, the initiative included a pre- and post-intervention survey, an educational handout summarizing American Society of Anesthesiologists temperature monitoring standards, laminated operating room reminders, and email communications. Retrospective data were analyzed using the Epic SlicerDicer tool to compare probe utilization and hypothermia incidence (defined as <35.5 °C) before and after the intervention. Following education, anesthesia provider awareness of esophageal probe accuracy increased from 40% to 45%, and perceived benefit rose from 56% to 65%. Esophageal probe use increased by 59% from 17 to 27 cases, while nasopharyngeal probe use increased by 218% from 27 to 86 cases. Although knowledge improved, practice patterns remained largely unchanged due to unclear probe selection criteria, limited in-person training, and documentation inconsistencies. These findings suggest that education alone may not sustain behavioral change; future initiatives should incorporate live training, clear criteria, and ongoing feedback.
Gerard Hogan
College of Applied Studies
Nurse Anesthesia Practice
ghogan@pc.fsu.edu
{Empty}
{Empty}
intraoperative hypothermia, esophageal temperature probe, nasopharyngeal temperature probe
{Empty}
Complete
Synchronous Online Presentation
No
2026
5th annual Undergraduate Research Symposium, April 17, 2025
https://pc.fsu.edu/student-research/symposium/research-symposium-program-portal?element_parents=elements/student_photo&ajax_form=1&_wrapper_format=drupal_ajax&token=KWuqPDGldqa6_e8xuE_jLWLvS2koh26wlyzrUyXZqGU
{Empty}

